

Glucose
All parts of the body need energy to work. Our main source of energy is glucose. Our body makes glucose from the food we eat and drink. Food molecules are broken down into sugars and absorbed in the small intestine then converted into glucose in the liver and circulated throughout the body.
Insulin
To be able to use glucose, your body needs insulin. This is a hormone made in the pancreas and enables the glucose in the blood to enter your body’s cells as it is needed.
Low levels of insulin constantly circulate throughout the body. When blood glucose levels rise after a meal, insulin is released by the pancreas.
Many of the body’s cells have insulin receptors on their surfaces. When insulin docks on to these receptors, signals are sent inside the cell and this allows glucose to enter.
A few hours after a meal, when your cells have taken up all the glucose they need and as a result, blood levels of glucose have fallen, insulin then signals to the liver to store the remaining excess blood glucose. It stores this as carbohydrates and fat.
Humans need insulin on a daily basis to survive. Without insulin, glucose cannot leave the bloodstream and enter the body's cells.
Type 2 diabetes
If you have diabetes, this system does not work as it should. People with type 1 diabetes produce very little or no insulin and must take insulin to control their blood glucose. In type 2 diabetes, the insulin you are making isn’t being taken up by your cells properly and your cells are not responding effectively to the insulin signal. This is a condition called insulin resistance.
When glucose can't get into your cells, your blood glucose levels rise. The pancreas tries to compensate by producing more insulin. Over time, this strains the pancreas and eventually it cannot make enough insulin. Long-term high blood glucose levels can cause progressive damage to body organs resulting in health problems like heart attacks and strokes, as well as damage to your eyes, kidneys, and feet.
People at greater risk of developing diabetes are those over 40 years of age and this risk increases as we get older. People with a family history of diabetes, those who are of Aboriginal and Torres Strait Islander decent, from the Pacific Islands, Indian subcontinent or Chinese cultural background are at a greater risk of developing diabetes.
Gestational diabetes and overt diabetes in pregnancy (DIP)
Diabetes in pregnancy means having diabetes while you are pregnant, and there are two types:
Fasting glucose
The fasting blood glucose test is used to screen for and diagnose diabetes. This measures the amount of glucose in your blood at the time you give the sample. To give a fasting blood sample you must not eat anything for eight to 12 hours beforehand. This is to ensure your blood is not affected by any recent food intake.
HbA1c
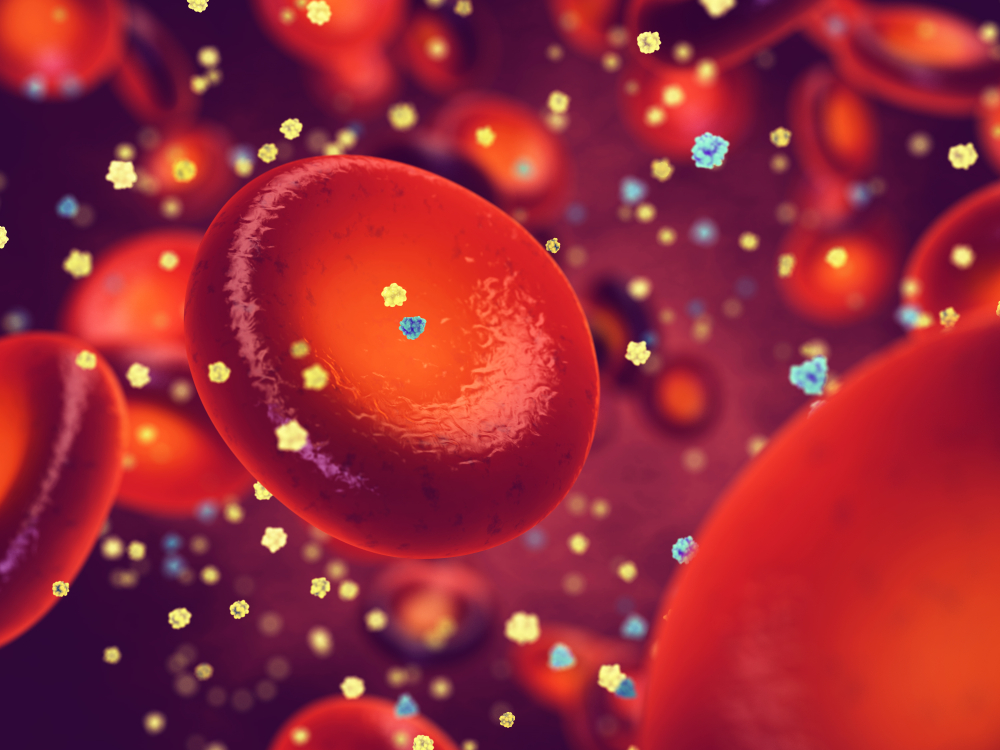
The HbA1c test can assess how well your glucose has been controlled over the previous few months. It does this by measuring the amount of haemoglobin in your blood that has an attached glucose molecule.
Glucose in your blood sticks to haemoglobin, the red protein in your red blood cells. As your blood glucose levels increase, more glucose attaches to your haemoglobin. Glucose sticks to haemoglobin for as long as the red blood cells are alive. Red blood cells live an average of about 120 days. Because of this, the test results can give you an average glucose level over the previous months. Click here for information on the HbA1c test.
Glucose tolerance test (GTT)
If your HbA1c and fasting glucose test results show that your blood glucose levels are too high, you will be asked to have a GTT. The GTT assesses how well your body uses glucose.
The test takes two hours to perform and begins with a fasting glucose test to establish a baseline glucose level. After this, you will be asked to take a glucose drink to challenge your system. One hour later, another blood sample is taken, and the blood sugar level is checked. Another hour later, it will be checked again. In this way it is possible to measure how quickly a dose of glucose is cleared from your blood.
Random glucose test
If you have diabetes you will need to monitor your own blood glucose levels. This is usually done by placing a drop of blood from a finger prick onto a plastic indicator strip and then inserting the strip into a glucose meter, which provides a digital readout of your blood glucose level.
Gestational diabetes
If you are pregnant, it is recommended that you be screened for gestational diabetes between your 24th and 28th week of pregnancy using a glucose tolerance test. If you are at higher risk (because you are older, overweight or have a history of gestational diabetes), you should be screened earlier.
Reading your test report
Your results will be presented along with those of your other tests on the same result form. You will see separate columns or lines for each of these tests.
What your results mean
High levels of glucose most often indicate diabetes, but many other health conditions can also cause raised glucose.
The following information is on the cutoff levels used to diagnose diabetes.
Fasting blood glucose
| Glucose level | What it means |
| From 3.0 - 6.0 mmol/L | Normal glucose tolerance |
| From 6.1 - 6.9 mmol/L | Impaired fasting glucose |
| 7.0 mmol/L and above | Probable diabetes |
Glucose tolerance test (GTT)
| Results 2 hours after a 75 gram glucose drink | |
| Glucose level | What it means |
| 3.0 - 7.7 mmol/L | Normal glucose tolerance |
| 7.8 - 11.0 mmol/L | Impaired fasting glucose |
| Equal to or more than 11.1 mmol/L | Probable diabetes |
Glucose tolerance test (GTT) during pregnancy
| Results 2 hours after a 75 gram glucose drink | |
| Time of sample | Gestational diabetes |
| Fasting (before the drink) | 5.1 mmol/L or greater |
| At one hour | 10.0 mmol/L or greater |
| At two hours | 8.5 mmol/L or greater |
The diagnosis of gestational diabetes is made if one or more of the above values are abnormal.
Click here for information on HbA1c test results.
Reference intervals
Your results will be compared to reference intervals (sometimes called a normal range).
If your results are flagged as high or low this does not necessarily mean that anything is wrong. It depends on your personal situation. Your results need to be interpreted by your doctor.
The choice of tests your doctor makes will be based on your medical history and symptoms. It is important that you tell them everything you think might help.
You play a central role in making sure your test results are accurate. Do everything you can to make sure the information you provide is correct and follow instructions closely.
Talk to your doctor about any medications you are taking. Find out if you need to fast or stop any particular foods or supplements. These may affect your results. Ask:
Pathology and diagnostic imaging reports can be added to your My Health Record.
You and your healthcare provider can now access your results whenever and wherever needed. Get further trustworthy health information and advice from healthdirect.