

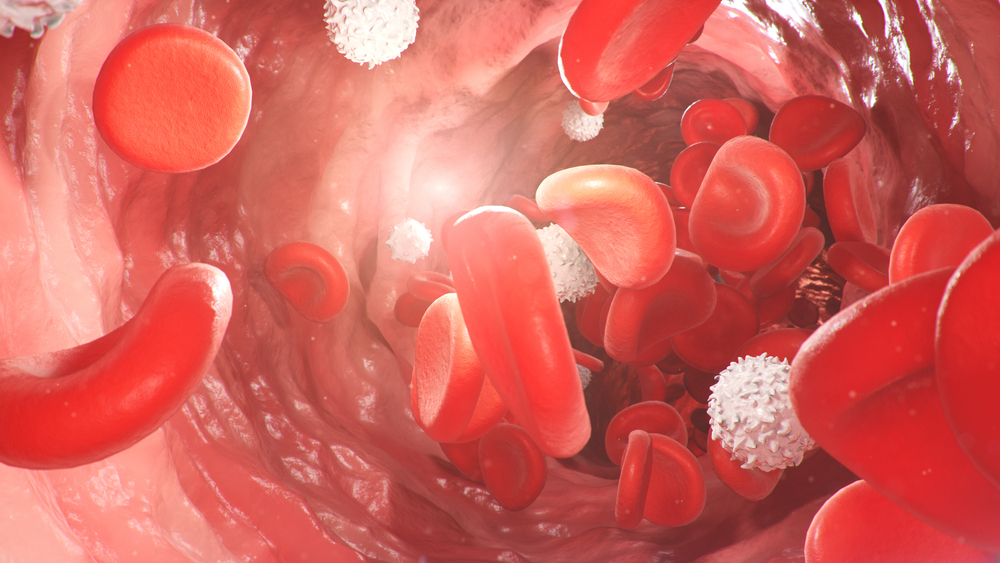
Your blood is made up of red blood cells (RBCs), white blood cells (WBCs) and platelets. These float in fluid called plasma.
RBCs are the most common type of blood cell – they make up almost half of your blood - and they play an essential role in carrying oxygen to every cell in your body. All cells in every part of your body need oxygen to make energy so that they can function properly.
In order to produce energy, oxygen combines with glucose, which you get from the food you eat. This process releases water and bicarbonate.
As a waste product, bicarbonate passes from the cells back into the blood where it is carried to your lungs to be breathed out as carbon dioxide.
RBCs can carry oxygen because they contain haemoglobin, the red protein that gives the blood its colour. Both oxygen and bicarbonate bind to the haemoglobin in RBCs so they can be transported.
How are red blood cells made?
Blood cells are made in your bone marrow, the soft fibrous tissue inside many of your bones. In order to stay healthy, your body must constantly make new blood cells to replace old ones. In general, RBCs have a lifespan of about 120 days.
New RBCs are produced as stem cells in the bone marrow. They develop through several stages into mature cells. RBCs stay in your bone marrow until they are needed and then are released into your blood. Mature RBCs are known as erythrocytes. They are round with a flattish, indented centre, like a doughnut without a hole.
The purpose of the RBC count is to find out if the number of RBCs you have is normal or abnormal. An RBC count is always included as part of a Full Blood Count (FBC) - a very common test that assesses the health status of all your blood.
Too few RBCs – anaemia
If the number of RBCs in your blood sample is 10 per cent under what is considered normal, you are said to be anaemic.
Too many RBCs – polycythaemia (erythrocytosis)
If you have too many RBCs you are said to have polycythaemia. This makes your blood thicker than it should be, and without treatment it could increase your risk of blood clots.
There are two types of polycythaemia. Primary polycythaemia is due to a bone marrow problem (myeloproliferative neoplasm) as in polycythaemia vera (PV). PV is a condition in which the bone marrow produces too many RBCs, along with high numbers of WBCs and platelets. It is caused by a variant or mutation in particular genes, especially the JAK2 gene which is responsible for making a protein that is needed to produce blood cells.
Secondary polycythaemia is more common and occurs when a health condition is preventing oxygen from getting to your tissues. This may be due to problems with lung function, heart function or rarely, due to problems with the kidneys or adrenal glands (small glands on your kidneys). Your body makes up for lower oxygen levels by making more blood cells that can carry more oxygen.
Tests that are used together with the RBC count
The results of other tests included in the FBC will be used to assess your RBCs.
Possible further tests for anaemia
Sample
Blood.
Any preparation?
None.
Reading your test report
Your results will be presented along with those of your other tests on the same form. You will see separate columns or lines for each of these tests.
| Low RBC count (anaemia) | High RBC count (polycythaemia) |
|
|
Reference intervals - comparing your results to the healthy population
Your results will be compared to reference intervals (sometimes called a normal range).
If your results are flagged as high or low this does not necessarily mean that anything is wrong. It depends on your personal situation.
Reference intervals for the RBC count vary between labs so you will need to go through your results with your doctor. Your doctor is the best person to interpret your results.
| Example reference intervals for Red Blood Cell Count | |
| Male | 4.35 – 5.65 trillion cells/L |
| Female | 3.92 – 5.13 trillion cells/L |
Reference intervals for RBC count can vary between laboratories. This is because labs use different instruments and chemical processes to analyse samples. The reference interval given here is used by many labs but not all. Women tend to have lower RBC counts than men, and levels tend to decrease with age. An RBC count measures the number of RBCs per litre of blood. | |
The choice of tests your doctor makes will be based on your medical history and symptoms. It is important that you tell them everything you think might help.
You play a central role in making sure your test results are accurate. Do everything you can to make sure the information you provide is correct and follow instructions closely.
Talk to your doctor about any medications you are taking. Find out if you need to fast or stop any particular foods or supplements. These may affect your results. Ask:
Pathology and diagnostic imaging reports can be added to your My Health Record. You and your healthcare provider can now access your results whenever and wherever needed.
Get further trustworthy health information and advice from healthdirect.