

Your body needs vitamin B12 (also known as cobalamin) and folate (also known as vitamin B9) to form and repair red blood cells, nerve cells and brain cells. They are also critical in making your DNA.
Your body does not make vitamin B12 or folate which means you must get them from your diet.
A healthy adult typically has enough B12 stored to last about three to five years. Since folate is stored in the body in smaller quantities than vitamin B12, it must be taken in more regularly.
How do B12 and folate deficiencies occur?
B12 and folate deficiencies occur when your body is either not getting enough through your diet or not absorbing enough because of a malabsorption disorder in your intestines.
Folate is especially important if you are pregnant when you need more B12 and folate to cater for the growing baby. Concerns over the link between folate deficiency in pregnancy and premature birth or neural tube disorders such as spina bifida led to mandatory folate fortification of flour, folate being added to all flour in Australia in the 1990s.
B12 and folate deficiencies can take months or even years to show up in adults whereas infants and children show signs of deficiency more quickly because they haven’t yet built up a store.
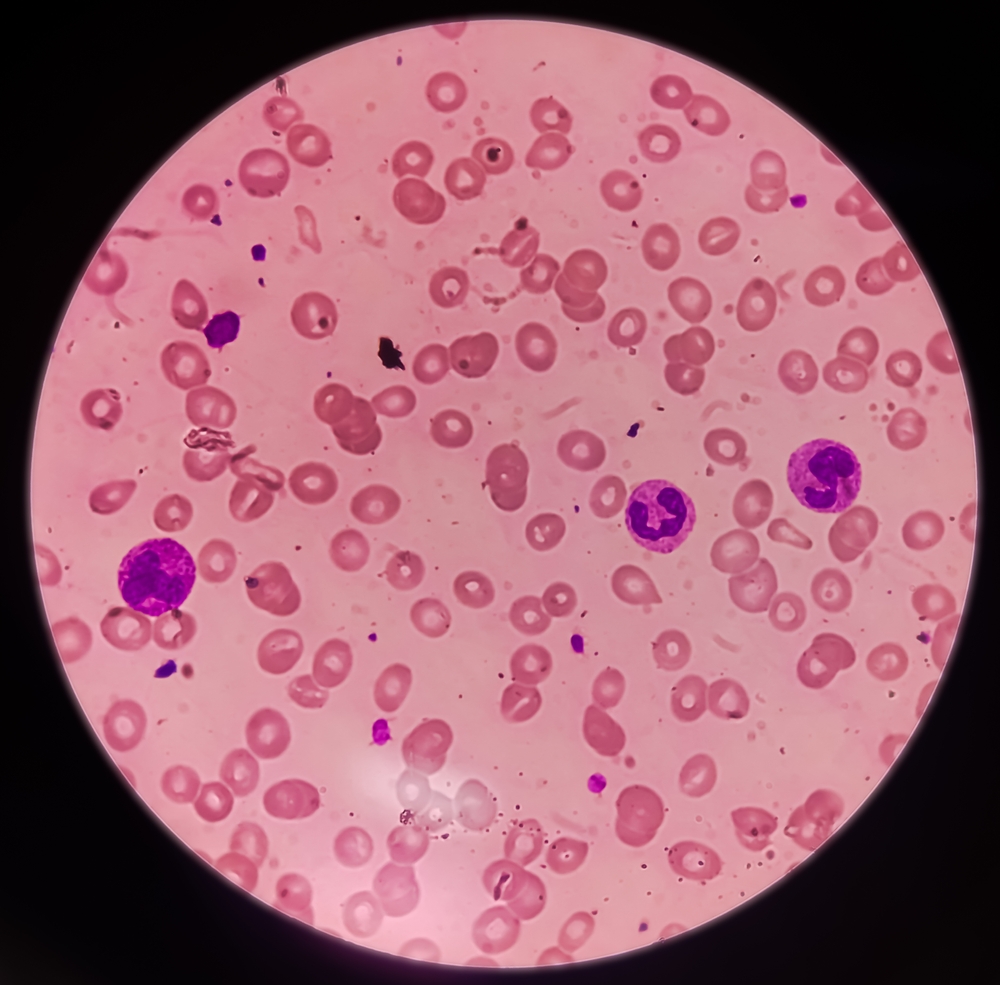
Over time, a lack of B12 and/or folate can lead to macrocytic anaemia. Macrocytic anaemia refers to having larger but fewer red blood cells.
One form of macrocytic anaemia is megaloblastic anaemia in which red blood cells aren’t formed properly in your bone marrow. Like all blood cells, red cells are made in the bone marrow. Your body needs a constant supply of new cells as old cells die off and are replaced. The average lifespan of a red blood cell is 120 days.
Vitamin B12 and folate are needed to make red blood cells. Without enough of them, your body produces abnormal cells called megaloblasts. These cells don’t reproduce like healthy cells, which means there are fewer red blood cells made. These abnormal cells are unusually large, so they don’t easily move into your bloodstream. They are unable to carry as much oxygen around the body as they should, and they die earlier than normal.
Left untreated this can lead to a range of health problems including neurological disorders – these are health problems that affect your nervous system. Symptoms can include:
People at risk of deficiency include:
Full Blood Count (FBC)
Vitamin B12 and folate tests are ordered if you have had an abnormal result from a Full Blood Count test that shows you have low haemoglobin levels, fewer but larger red blood cells and abnormal white blood cells.
Haemoglobin is the red protein in red blood cells containing iron that is needed for carrying oxygen around the body. Unusually large red blood cells will be shown by the mean corpuscular volume (MCV) part of the Full Blood Count. This measures the average size of your red blood cells. The result of this test will be high when your red blood cells are larger than normal (macrocytic).
Total vitamin B12 and serum folate
The first tests that will be ordered to investigate B12 and folate deficiencies are total vitamin B12 and serum folate. Serum is the thin yellowish liquid part of the blood.
It is possible for some people to have a deficiency in B12 and folate yet have normal test results. This is more likely to be the case if you also have iron deficiency.
Active B12 (holotranscobalamin)
Measuring B12 and folate levels in blood serum cannot show how much of the vitamins are in your tissues.
In the past, a test that measured folate in red blood cells was used to assess longer-term vitamin storage as this reflected the amount of folate stored in the body’s tissues over the lifetime of red blood cells – about 120 days. Red blood cell folate testing is no longer used.
More recently, another test has been made available on Medicare (from July 2025) that is more accurate. This measures Active B12 also known as holotranscobalamin (HoloTC).
About 25 per cent of circulating B12 binds to a protein called transcobalamin so that it can be taken up by the cells of the body. For this reason, it is referred to as the active form of B12.
Measuring this form of B12 is considered the best measure of B12 in the body. This test can be ordered together with a total vitamin B12 and serum folate test to give a complete picture.
Intrinsic factor antibodies and parietal cell antibodies
Intrinsic factor is a protein produced by cells in the lining of the stomach wall known as parietal cells. During digestion, stomach acids release vitamin B12 from food and bind to intrinsic factor. In pernicious anaemia the immune system makes antibodies against these cells.
Identifying intrinsic factor antibodies and parietal cell antibodies may be helpful in investigating whether you have pernicious anaemia, but there are limitations to the sensitivity and specificity of these tests. Any B12 treatment you have had within two weeks of the sample being collected could interfere with results of these tests.
Homocysteine
Homocysteine is a chemical in your blood that helps build proteins. This test measures the level of homocysteine in the blood. B12 and folate are needed to break down homocysteine, and this keeps homocysteine levels low. Therefore, people who are deficient in B12 and folate may have increased levels of homocysteine.
While a normal homocysteine level in your blood makes B12 and folate deficiencies unlikely, higher homocysteine levels can often be seen in the elderly or people with kidney disease who have normal B12 and folate levels.
Sample
Blood.
Test preparation?
Ask your doctor for specific instructions. You may be asked to fast before blood sample collection especially for serum folate testing. Biotin found in some supplements can interfere with testing. Certain medicines can also affect the test results.
Reading your test report
Your results will be presented along with those of your other tests on the same form. You will see separate columns or lines for each of these tests.
| Result | Interpretation |
| Normal B12 and folate levels | This may mean that you do not have a deficiency and that your symptoms are due to another cause. However, normal levels may reflect the fact that your stored B12 and/or folate have not yet been fully depleted. |
| If you have a normal or low-normal B12 result but a deficiency is still suspected | B12 and folate tests cannot tell you the severity of a deficiency or the cause. You may need further tests to see what’s causing your symptoms. |
| Low B12 and/or folate levels | This means that you have a deficiency, and further tests need to be done to investigate the underlying cause. |
| High levels of B12 | This is uncommon and not usually clinically monitored. Someone with chronic myeloproliferative neoplasm, diabetes, heart failure, obesity, AIDS or severe liver disease, may have an increased vitamin B12 level. Taking oestrogens, vitamin C or vitamin A can also cause high B12 levels. |
Reference intervals
Your results will be compared to reference intervals (sometimes called a normal range).
If your results are flagged as high or low this does not necessarily mean that anything is wrong. Your doctor needs to take your medical history to help interpret your result.
Medicare provides a rebate for a Total vitamin B12 test once every 12 months, in line with current best practice. As of July 2025, Active B12 (holotranscobalamin) is also available as a first-line test.
The choice of tests your doctor makes will be based on your medical history and symptoms. It is important that you tell them everything you think might help.
You play a central role in making sure your test results are accurate. Do everything you can to make sure the information you provide is correct and follow instructions closely.
Talk to your doctor about any medications you are taking. Find out if you need to fast or stop any foods or supplements. These may affect your results. Ask:
Pathology and diagnostic imaging reports can be added to your My Health Record. You and your healthcare provider can now access your results whenever and wherever needed.
Get further trustworthy health information and advice from healthdirect.