What is being tested?
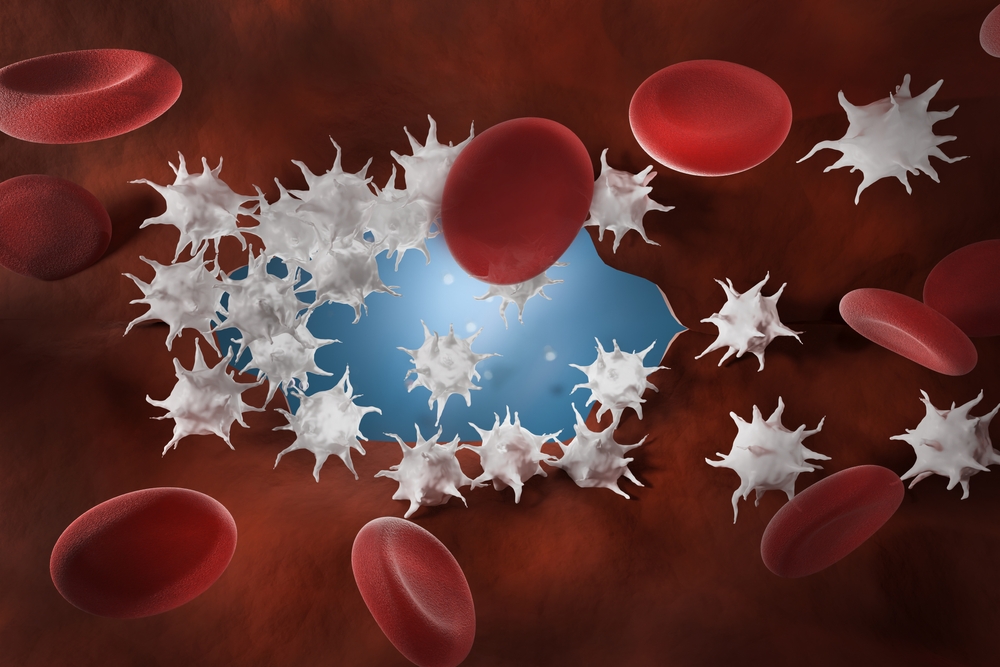
Antithrombin testing measures the function and quantity of antithrombin. Antithrombin is a protein produced by the liver to help control blood clotting. Normally, when a blood vessel is injured, the body activates a series of coagulation factors, in a process called the coagulation cascade, to form a blood clot and prevent further blood loss. Antithrombin helps to regulate this process by inhibiting the action of several activated coagulation factors, including thrombin and factors Xa, IXa, and XIa, to slow down the process and prevent excessive or inappropriate clotting.
Patients with inherited or acquired antithrombin deficiency are at increased risk of venous thrombosis. Inherited deficiencies are rare (about 1 in 5000 patients). If a person has one defective gene and one normal gene (heterozygous), then inappropriate clotting episodes typically start at about 20 to 30 years of age. Very rarely, an individual has two defective antithrombin genes, resulting in severe thrombotic problems soon after birth.
Acquired antithrombin deficiencies may occur at any age. They are associated with a variety of conditions, including liver disease, extensive thrombosis, disseminated intravascular coagulation (DIC), blood loss, cancer, and nephrotic syndrome – a form of kidney disease.
There are two types of antithrombin deficiency. With type 1, normal antithrombin is produced, but the quantity made is insufficient. With type 2, there is a sufficient quantity of antithrombin produced, but it is dysfunctional. These types can be detected, differentiated and assessed using two antithrombin tests. They are:
How is it used?
Antithrombin testing is primarily ordered, along with other tests for hypercoagulable disorders, to investigate the cause of recurrent venous thrombosis. The antithrombin activity test is performed before the antigen test, to evaluate whether the total amount of functional antithrombin is normal. Activity will be decreased with both type 1 and type 2 antithrombin deficiencies, so this test can be used as an initial screen for both. If the antithrombin activity is low, then the antithrombin antigen test is performed to determine the quantity of antithrombin present. If a deficiency is detected, both antithrombin tests are repeated at a later date to confirm test findings. Antithrombin testing may be used to evaluate patients not responding as expected to heparin.
When is it requested?
Antithrombin activity testing is ordered, along with other tests for hypercoagulable disorders (such as protein C and protein S, and lupus anticoagulant), when a patient has been experiencing recurrent venous thrombosis. Antithrombin should be measured after a blood clot has been treated and resolved as both the presence of the clot, and the therapy used to treat it, will affect antithrombin results.
Antithrombin testing may be ordered when a patient is not responding as expected to heparin anticoagulation - when unusually high doses of heparin are necessary to achieve the desired level of anticoagulation.
What does the result mean?
Decreased antithrombin activity and decreased quantities of antithrombin antigen suggest a type 1 antithrombin deficiency. In this case, the activity is decreased because there is less antithrombin available to participate in clotting regulation. Reduced antithrombin activity and normal levels of antithrombin antigen suggest a type 2 antithrombin deficiency. This means that there is sufficient antithrombin, but it is not functioning as it should.
If the antithrombin activity is normal, then the antithrombin antigen test is usually not performed. In this case, the antithrombin is functioning adequately and the recurrent thrombotic episodes being investigated are likely due to another cause.
Increased levels of antithrombin are not usually considered a problem. They may be seen with:
Testing for antithrombin deficiency is not recommended unless the patient’s condition is stable. Temporarily or chronically decreased antithrombin levels may be seen with conditions that affect its consumption or production, such as:
Is there anything else I should know?
If a patient with an antithrombin deficiency also has other coagulation risks, such as a protein C or S deficiency, a factor V mutation (Leiden), or oral contraceptive use, then they may be at a significantly elevated risk of developing a blood clot.
Antithrombin deficiency may possibly increase the risk of recurrent miscarriage.
Patients with antithrombin deficiency may need to take preventative anticoagulation prior to medical or surgical procedures.
Antithrombin concentrates may be used to temporarily correct acute or chronic antithrombin deficiencies.
Common questions
If you have a personal or strong family history of recurrent blood clots, your doctor may do a physical to determine your general state of health and order a series of tests to determine your risk of having a hypercoagulable disorder. The more inherited or acquired risk factors you have (such as a Factor V mutation (Leiden), PT 20210 mutation, or a Protein C or S deficiency), the higher your relative risk of clotting. This risk can be further increased if you are overweight, sedentary, have hypertension, smoke and/or take oral contraceptives. It is important to remember, however, that any overall relative risk that is determined is still a statistical risk. No one can predict whether a particular patient will actually experience recurrent clotting.
Yes. This is important information that your health care providers should know about as it affects your body’s ability to clot appropriately during and after a medical procedure which may increase the risk of forming a blood clot.
More information
What is Pathology Tests Explained?
Pathology Tests Explained (PTEx) is a not-for profit group managed by a consortium of Australasian medical and scientific organisations.
With up-to-date, evidence-based information about pathology tests it is a leading trusted source for consumers.
Information is prepared and reviewed by practising pathologists and scientists and is entirely free of any commercial influence.