What is being tested?
The Endocrine Society recommends that a test for plasma free metanephrine or urine metanephrine be used to help detect the presence of phaeochromocytomas and paragangliomas (catecholamine-secreting tumours). Urine and/or blood tests for catecholamines may be used to help confirm or rule out the presence of these tumours.
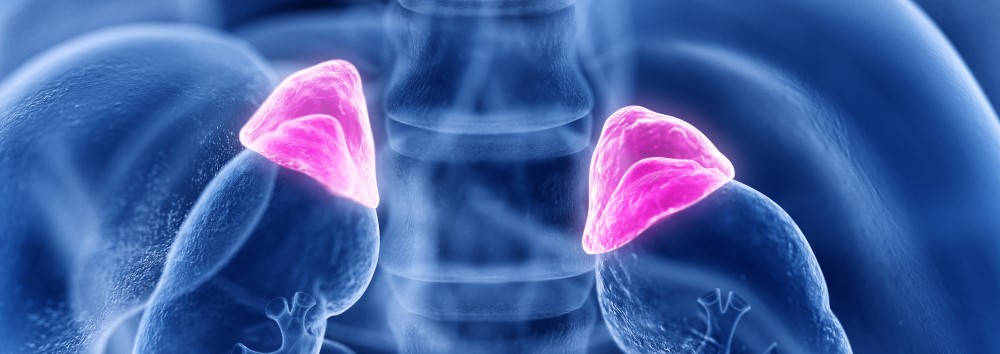
Catecholamines are a group of similar hormones produced in the medulla (central portion) of the adrenal glands. The adrenal glands are small, triangular organs located on top of each kidney. The primary catecholamines are dopamine, adrenaline (epinephrine) and noradrenaline (norepinephrine). These hormones are released into the bloodstream in response to physical or emotional stress. They help transmit nerve impulses in the brain, increase glucose and fatty acid release (for energy), dilate bronchioles (small air passages in the lungs) and dilate the pupils. Noradrenaline also constricts blood vessels (increasing blood pressure) and adrenaline increases heart rate and metabolism.
After completing their actions, the hormones are metabolised to form inactive compounds. Dopamine becomes homovanillic acid (HVA), noradrenaline breaks down into normetanephrine and hydroxymethylmandelic acid (HMMA) (vanillylmandelic acid (VMA)), and adrenaline becomes metanephrine and HMMA. Both the hormones and their metabolites are excreted in the urine.
Normally, catecholamines and their metabolites are present in the body in small, fluctuating amounts that only increase appreciably during and shortly after a bout of stress. Catecholamine-secreting tumours (phaeochromocytomas and paragangliomas), however, can produce large amounts of catecholamines, resulting in greatly increased concentrations of the hormones and their metabolites in both the blood and urine. This can cause persistent hypertension (high blood pressure) and/or bouts or episodes of severe hypertension, resulting in symptoms such as severe headaches, palpitations, sweating, nausea, anxiety and tingling in the extremities.
While a few are cancerous, most are benign (they do not spread beyond their original location ) although most do continue to grow. Left untreated, the symptoms may worsen as the tumour grows and, over a period of time, the hypertension that the tumour causes may damage body organs, such as the kidneys and heart, and raise the risk of an affected patient having a stroke or heart attack.
Urine and plasma catecholamine testing can be used to help detect the presence of catecholamine-secreting tumours. It is important to diagnose and treat these rare tumours because they cause a potentially curable form of hypertension. In most cases, the tumours can be surgically removed and/or treated to significantly reduce the amount of catecholamines being produced and to reduce or eliminate their associated symptoms and complications.
Catecholamine testing measures the amount of adrenaline, noradrenaline and dopamine in the plasma or urine. (The metabolites of these hormones may be measured separately with a urine metanephrine and/or HMMA test). The plasma catecholamine test measures the amount of hormones present at the moment of collection, while the urine test measures the amount excreted over a 24-hour period.
How is it used?
Catecholamine testing is primarily used to help detect and rule out catecholamine-secreting tumours in symptomatic patients. It also may be ordered to help monitor the effectiveness of treatment when a catecholamine-secreting tumour is discovered and removed and to monitor for recurrence. The plasma test is most useful when the patient has persistent hypertension or is currently experiencing an episode of hypertension. This is because the hormones do not linger in the blood; they are used by the body, metabolised, and/or excreted. Urine catecholamine testing measures the total amount of catecholamines released in 24 hours. Since the hormone levels may fluctuate significantly during this period, the urine test may detect excess production that is missed with the blood test. Plasma and urine tests may be ordered together or separately and/or along with urine and/or plasma metanephrines to look for excessive amounts of both catecholamines and their metabolites.
Since these tests are affected by drugs, foods and stresses, there will be a certain number of false positives. For this reason, catecholamine testing is not recommended as a screen for the general public. Doctors will frequently investigate a positive result by evaluating a patient’s stresses and intake, work to alter or minimise any influences, and then repeat the test to confirm the original findings.
Occasionally, the tests may be ordered on an asymptomatic person if an adrenal or neuroendocrine tumour is detected during a scan that is done for another purpose or if the patient has a strong personal or family history of these tumours (as they may recur and there is a genetic link in some cases).
When is it requested?
Catecholamine testing may be ordered when tests for plasma free metanephrines and/or urine metanephrines are inconclusive and a health practitioner needs more information about a possible catecholamine-secreting tumor. A Doctor may order it when a patient has persistent or recurring hypertension along with symptoms such as headaches, sweating, flushing and rapid heart rate. It may also be ordered when a patient has hypertension that is not responding to treatment (patients with a phaeochromocytoma are frequently resistant to conventional therapies).
Occasionally, the test may be ordered when an adrenal tumour or neuroendocrine tumour is detected incidentally or when a patient has a family history of phaeochromocytomas. It may also be used as a monitoring tool when a patient has been treated for a previous .
What does the result mean?
Since the catecholamine test is sensitive to many outside influences and catecholamine-secreting tumours are rare, a doctor may see more false positives with this test than true positives. If a symptomatic patient has large amounts of catecholamines in her blood and/or urine, further investigation is indicated. Serious illnesses and stresses can cause moderate to large temporary increases in catecholamine levels. Doctors must evaluate the patient as a whole - his or her physical condition, emotional state, medications and diet. When interfering substances and/or conditions are found and resolved, the doctor will frequently re-test the patient to determine whether the catecholamines are still elevated. The doctor may also order blood and/or urine metanephrine testing to help confirm his findings and imaging tests (such as an MRI scan) to help find the tumour(s).
If levels are elevated in a patient who has had a previous catecholamine-secreting tumour, then it is likely that either treatment was not fully effective or that the tumour is recurring.
Catecholamine-secreting tumours do not necessarily produce catecholamines at a constant rate, however. If the patient has not had a recent paroxysm of hypertension, their plasma and urine concentrations of catecholamines could be at normal or near normal levels even when a catecholamine-secreting tumour is present.
Is there anything else I should know?
While plasma and urine catecholamine testing can help detect and diagnose catecholamine-secreting tumours, they cannot tell the doctor where the tumour is, whether there is more than one, or whether or not the tumour is benign (although most are). The amount of catecholamines produced does not necessarily correspond to the size of the tumour. This is a physical characteristic of the tumour tissue. The total amount of catecholamines produced will tend to increase, however, as the tumour increases in size.
It is very important to talk to your doctor before discontinuing any prescribed medications. He will work with you to identify interfering substances and drug treatments to determine which of them can be safely interrupted and which must be continued for your well-being.
Some of the substances that can interfere with catecholamine testing include: paracetamol (acetaminophen), aminophylline, amphetamines, appetite suppressants, coffee, tea, and other forms of caffeine, chloral hydrate, clonidine, dexamethasone, diuretics, adrenaline, ethanol (alcohol), insulin, imipramine, lithium, methyldopa, MAO (monoamine oxidase) inhibitors, nicotine, nitroglycerine, nose drops, propafenone, reserpine, salicylates, theophylline, tetracycline, tricyclic antidepressants and vasodilators.
The effects of these drugs on catecholamine results will be different from patient to patient and are often not predictable. Bananas and capsicums may also cause falsely elevated catecholamine results and should be avoided for 24 hours before and during the urine collection.
Common questions
No, they can be detected and removed but not prevented. In most cases, the tumour is benign and, once it is removed, it will not recur.
No, testing must be done on specialised machines in a laboratory.
Yes, for accurate test results it is essential that all of the urine be collected. Because catecholamines are released at varying times, the one sample not included might be the one with the most hormones in it.
Yes because catecholamines are released from the adrenal glands in response to stress. If you are anxious or afraid, your catecholamines concentrations may be increased.
More information
What is Pathology Tests Explained?
Pathology Tests Explained (PTEx) is a not-for profit group managed by a consortium of Australasian medical and scientific organisations.
With up-to-date, evidence-based information about pathology tests it is a leading trusted source for consumers.
Information is prepared and reviewed by practising pathologists and scientists and is entirely free of any commercial influence.