What is being tested?
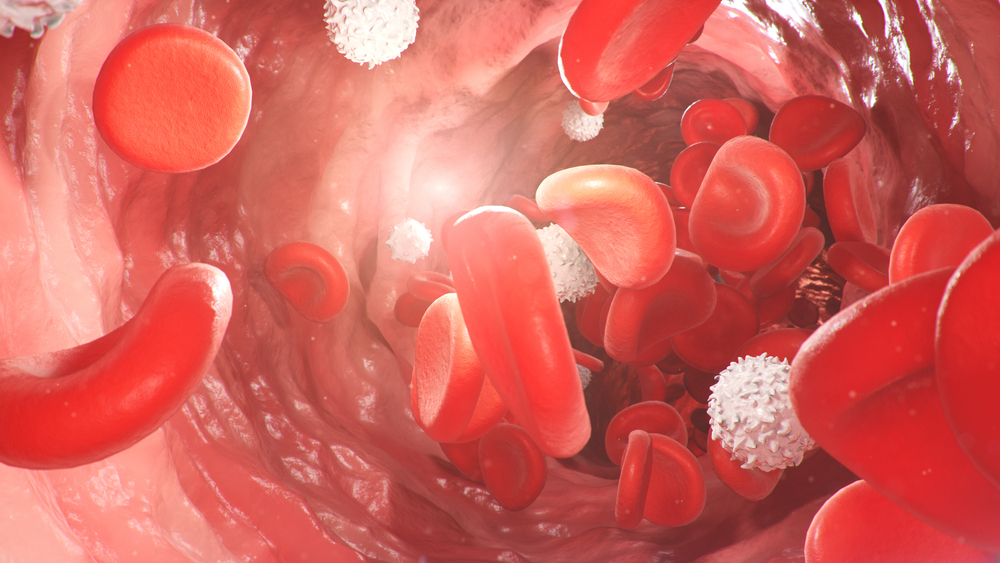
Erythrocyte sedimentation rate (ESR) is an indirect measure of the degree of inflammation present in the body. It measures the rate of fall (sedimentation) of erythrocytes (red blood cells) in a tall, thin tube of blood. Results are reported as how many millimetres of clear plasma are present at the top of the column after one hour. Normally, red cells fall slowly, leaving little clear plasma. Increased blood levels of certain proteins (such as fibrinogen or immunoglobulins, which are increased in inflammation) cause the red blood cells to fall more rapidly, increasing the ESR. In large laboratories the ESR may be performed by an automated analyser.
How is it used?
The ESR is an easy, inexpensive, non-specific test that has been used for many years to help diagnose conditions associated with acute and chronic (that is, short or long duration) inflammation, including infections, cancers and autoimmune diseases. The ESR is said to be non-specific because increases do not tell the doctor exactly where the inflammation is in your body or what is causing it, and also because it can be affected by other conditions besides inflammation. For this reason, an ESR is typically used in conjunction with other tests (see Common questions).
The ESR is helpful in diagnosing two specific inflammatory diseases, temporal arteritis and polymyalgia rheumatica. A high ESR is one of the main test results used to confirm the diagnosis. It is also used to monitor disease activity and response to therapy in both of these diseases.
When is it requested?
A physician usually requests an ESR test (along with other tests) to evaluate a patient who has symptoms that suggest polymyalgia rheumatica or temporal arteritis, such as headaches, neck or shoulder pain, pelvic pain, anaemia, unexplained weight loss and joint stiffness. There are many other conditions that can result in a temporary or sustained elevation in the ESR and some that will cause a decrease.
Since the ESR is a non-specific marker of inflammation and is affected by other factors, the results must be used along with the doctor’s other clinical findings, the patient’s health history, and results from other appropriate laboratory tests. If the ESR and clinical findings match, the doctor may be able to confirm or rule out a suspected diagnosis. A single elevated ESR, without any symptoms of a specific disease, will usually not give the doctor enough information to make a medical decision.
Before doing an extensive investigation looking for disease, a doctor may want to repeat the ESR test after a period of several weeks or months. If a doctor already knows the patient has a disease, like temporal arteritis (where changes in the ESR mirror those in the disease process), they may use the ESR at regular intervals to assist in monitoring the course of the disease.
What does the result mean?
Doctors do not base their decisions solely on ESR results. You can have a normal result and still have a problem.
A markedly elevated ESR may be associated with infections (including tuberculosis and other generalised infections), inflammation (temporal arteritis and polymyalgia rheumatic) and some cancers (multiple myeloma and other blood cancers in particular).
A Moderately elevated ESR may be seen in the above conditions, but also more commonly occurs with inflammatory arthritis, anaemia, aging and pregnancy.
A rising ESR can mean an increase in inflammation or a poor response to a therapy; a decreasing ESR may be used to confirm a satisfactory response to therapy.
Although a low ESR is not usually important, it can be seen with polycythaemia (a condition where a patient makes too many red blood cells), with extreme leucocytosis (patient has too many white blood cells), and with some protein abnormalities.
Is there anything else I should know?
The ESR and C-reactive protein (CRP) are both markers of inflammation. Generally, ESR does not change as rapidly as does CRP, either at the start of inflammation or as it goes away. CRP is not affected by as many other factors as is ESR, making it a better marker of some types of inflammation. However, because ESR is an easily performed test and CRP must be done using sophisticated laboratory equipment, many doctors still use ESR as an initial test when they think a patient has inflammation.
Females tend to have a slightly higher ESR, and menstruation and pregnancy can cause temporary elevations.
Drugs such as dextran, methyldopa (Aldomet), oral contraceptives, penicillamine procainamide, theophylline and vitamin A can increase ESR, while aspirin, steroids and quinine may decrease it.
Common questions
Your doctor may request a CRP test as well as other biochemistry tests, and an FBC, at the same time they order an ESR. They may also request additional tests based on your symptoms, such as the ANA (antinuclear antibody) and RF (rheumatoid factor) tests suggestive of autoimmune diseases, or cultures to investigate infection. Serum electrophoresis can look for evidence of diseases such as multiple myeloma and lymphoma.
The ESR is an indicator in your body. Like pain, it is giving you a warning that something is wrong. In most cases, the ESR will decrease over time once the underlying inflammation is addressed. If you have a chronic (longstanding) inflammatory disease, the ESR may fluctuate with the degree of activity your condition.
What is Pathology Tests Explained?
Pathology Tests Explained (PTEx) is a not-for profit group managed by a consortium of Australasian medical and scientific organisations.
With up-to-date, evidence-based information about pathology tests it is a leading trusted source for consumers.
Information is prepared and reviewed by practising pathologists and scientists and is entirely free of any commercial influence.