What is being tested?
Luteinising hormone (LH) is produced by the pituitary gland in the brain. Control of LH production is a complex system involving hormones produced by the gonads (ovaries or testes), the pituitary gland and the hypothalamus, such as gonadotrophin-releasing hormone (GnRH).
Women’s menstrual cycles are divided into 2 phases, the follicular and luteal, by a mid-cycle surge of follicle-stimulating hormone (FSH) and LH. The high level of LH (and FSH) at mid-cycle triggers ovulation (release of the egg from the ovary). LH also stimulates the ovaries to produce other hormones, oestradiol and progesterone. Oestradiol helps the pituitary gland to control the production of LH. At the time of the menopause, the ovaries stop functioning and LH levels rise.
In men, LH stimulates the Leydig cells in the testes to produce testosterone. LH levels are relatively constant in men after puberty.
In infants and children, LH levels rise shortly after birth and then fall to very low levels (by 6 months in boys and 1-2 years in girls). At about 6-8 years, levels again rise with the beginning of puberty and the development of secondary sexual characteristics.
How is it used?
LH is often used in conjunction with other tests (FSH, testosterone, oestradiol and progesterone) in the investigation of infertility in both men and women. LH levels are also useful in the investigation of menstrual irregularities (irregular periods) and to aid in the diagnosis of pituitary gland disorders. In children, FSH and LH are used to diagnose delayed and precocious (early) puberty.
When is it requested?
In women and men, LH (along with FSH) is requested as part of the investigation of infertility and pituitary disorders.
LH and FSH may be measured when a boy or girl does not appear to be entering puberty at an appropriate age (either too late or too soon).
What does the result mean?
In women, FSH and LH levels can help to tell the difference between primary ovarian failure (failure of the ovaries themselves) and secondary ovarian failure (failure of the ovaries due to disorders of either the pituitary gland or the hypothalamus in the brain). Increased levels of FSH and LH are consistent with primary ovarian failure. Some causes of primary ovarian failure are listed below.
Developmental defects:
Premature ovarian failure due to:
Chronic anovulation (failure to ovulate) due to:
When a woman enters the menopause and her ovaries stop working, FSH and LH levels will rise.
Low levels of FSH and LH are consistent with secondary ovarian failure due to a pituitary or hypothalamic problem.
In men, high FSH levels are due to primary testicular failure. This can be due to developmental defects in testicular growth or to testicular injury, as indicated below.
Developmental defects:
Testicular failure:
Low levels of FSH are consistent with pituitary or hypothalamic disorders.
In young children, high levels of FSH and LH and development of secondary sexual characteristics at an unusually young age are an indication of precocious (early) puberty. This is much more common in girls than in boys.
Is there anything else I should know?
LH results can be increased with use of certain drugs, such as clomiphene and naloxone. LH results can decrease with oral contraceptives (the pill), phenothiazines and certain hormone treatments.
Common questions
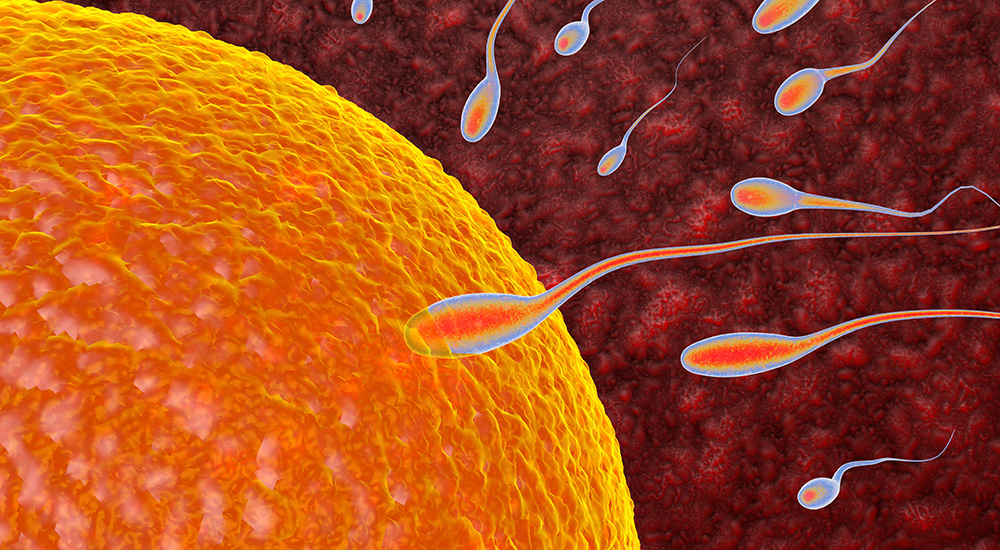
The basic test for infertility is measurement of progesterone to check that ovulation is occurring. Other tests for infertility include FSH and LH and other blood tests to assess your reproductive hormone levels. A post-coital test may be carried out where the cervical mucus is examined 2-8 hours after intercourse to check if the sperm are surviving in it. A hysterosalpingogram (image of fallopian tubes) may be done to see whether your fallopian tubes are blocked. Your partner may be asked to give a specimen of semen for analysis.
You may have polycystic ovary syndrome (PCOS), a hormonal problem seen in 5-10% of women of childbearing age and a major cause of infertility. With this condition, ovaries may become larger because of cysts that form in them. Women with PCOS also may have high levels of testosterone and do not ovulate normally. You may need to undergo several laboratory tests, including FSH, LH and testosterone, to make sure that PCOS is the condition causing your symptoms. A combination of medications and hormone therapy may help your symptoms.
Men also produce FSH and LH in their bodies, and these hormone levels are important for male reproduction too. In men, FSH stimulates the testes to produce sperm just as in women FSH stimulates the ovaries to produce eggs. In men, LH can be measured to investigate the cause of a low testosterone.
What is Pathology Tests Explained?
Pathology Tests Explained (PTEx) is a not-for profit group managed by a consortium of Australasian medical and scientific organisations.
With up-to-date, evidence-based information about pathology tests it is a leading trusted source for consumers.
Information is prepared and reviewed by practising pathologists and scientists and is entirely free of any commercial influence.