What is being tested?
Rubella is a viral infection that causes a fine red rash and flu-like symptoms, such as a high temperature, headache and a general feeling of being unwell. The raised red rash appears first on the face and neck and travels to the body and limbs. Teenagers and adults may experience more severe symptoms, such as joint pains, which may last several weeks. Rubella usually improves quickly without any special treatment. However if a woman gets rubella in the first three months of her pregnancy, serious birth defects, miscarriage or stillbirth may result.
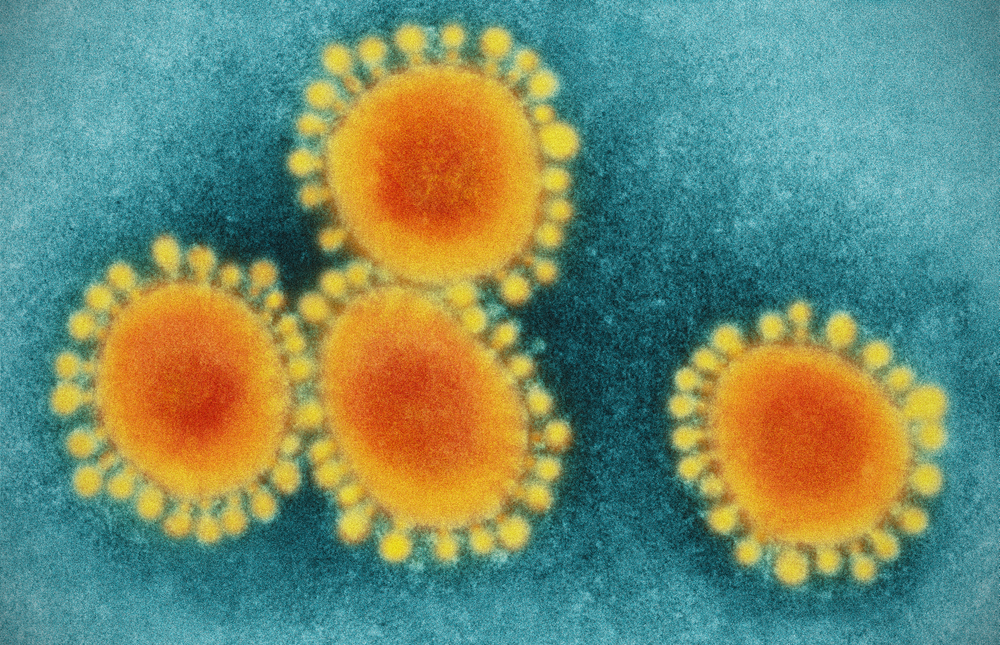
You are infected when you come into contact with the nasal or throat secretions of someone who has an active viral infection. If you catch rubella, you are infectious one week before the rash appears and one week after. In children, rubella infections generally produce mild symptoms. The number of new cases of rubella is low in Australia since a combined vaccine for measles, mumps, and rubella (MMR) is recommended for all children.
The test, which can be done at any time, will provide the necessary information about a person’s immunity to the virus.
How is it used?
A blood test can determine if you have had a recent or past infection, or if you have never been exposed to the rubella virus. People with recent infection or vaccination will have a positive IgM antibody and those with a past infection (and those who have been vaccinated for rubella) will have a positive IgG antibody. Neither antibody will be present if there has been no contact with the virus or vaccine. A blood test for both antibody types will help the doctor predict if you are protected from infection or if you are at risk.
When is it requested?
If you are pregnant and have exposure to a person with a rubella-like rash and flu-like symptoms or you develop a rash and symptoms, your doctor should request a laboratory test to help diagnose possible rubella infection. It is a particularly important to test for rubella in early pregnancy as infection during the first 16 weeks of pregnancy presents major risks for the unborn baby. Antibody testing is strongly recommended for women planning a pregnancy so those who are not immune to the virus can be vaccinated before they conceive. Antibody testing is often used in infants born with abnormalities, such as deafness, mental retardation, heart defects, and cataracts that may have resulted from a rubella infection acquired before their birth.
Testing for rubella antibody is not usually done on children or adults who were vaccinated to prove the vaccine was effective.
What does the result mean?
In an adult or child, the absence of IgG antibodies to rubella means the person is not immune. Absence of IgM antibodies and presence of IgG antibodies indicates a history of past exposure to the virus or vaccination. Presence of IgM antibodies with or without IgG antibodies usually represents recent infection. In an infant the presence of IgM antibodies means the baby was infected during the pregnancy. Occasionally, low levels of IgM antibodies represent a false positive result. A positive IgM result, particularly in pregnancy, needs to be interpreted with care.
Oral secretions or a throat swab are tested by a different technique looking for the presence of rubella virus, not the body's response to infection.
Is there anything else I should know?
If only a low level of antibodies are detected then the test may be inconclusive, and immunisation with the rubella vaccine may be recommended as a precaution.
In addition to antibody tests, the evidence of recent rubella infection is a positive viral culture for rubella or detection of rubella virus by testing for the genetic material (RNA) of the rubella virus in a body fluid sample, such as a throat swab. Because these procedures are complex, time-consuming and expensive, most diagnostic laboratories refer this testing to a reference laboratory.
Common questions
The rubella vaccine should not be given to a pregnant woman, and a woman should avoid getting pregnant for one month after taking the vaccine.
The vaccine contains a live virus that has been altered so it cannot cause all the problems associated with a natural infection. The most common side-effects are pain at the site of injection, fever, swollen glands or a rash following immunisation. Young children have a slightly increased risk of febrile convulsions up to 2 weeks following vaccination. Adults in particular may develop transient pain in their joints, especially their hands and wrists. There is no credible evidence linking the measles, mumps, rubella (MMR) vaccine to autism.
There is no antibiotic or anti-viral drug that can prevent or ‘cure’ the infection or reduce the risk of rubella to an unborn baby. Specialist advice is essential.
If you are going to have symptoms, the rash usually begins 15–17 days after coming in contact with an infectious person, but it may take as long as 3 weeks
What is Pathology Tests Explained?
Pathology Tests Explained (PTEx) is a not-for profit group managed by a consortium of Australasian medical and scientific organisations.
With up-to-date, evidence-based information about pathology tests it is a leading trusted source for consumers.
Information is prepared and reviewed by practising pathologists and scientists and is entirely free of any commercial influence.