What is being tested?
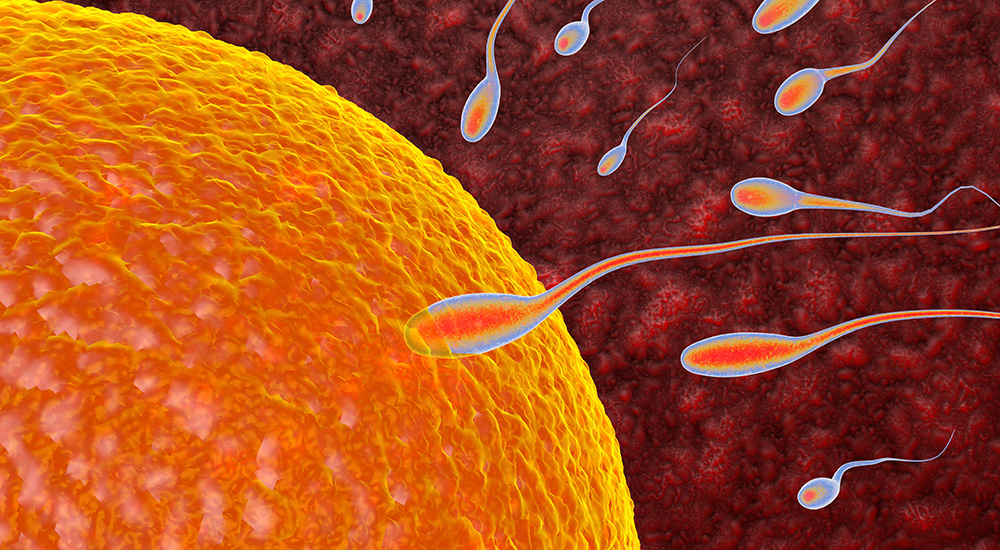
A semen analysis measures the quantity and quality of both the liquid portion, called semen, and the microscopic moving cells called sperm. Semen is the turbid, whitish substance that is released from the penis during ejaculation. Sperm are the cells in semen with a head and a tail that enables them to travel to the egg. A typical semen analysis could measure:
Additional tests may be performed if semen is abnormal, such as a test for sperm antibodies. If assisted reproductive technology is contemplated, for example, in vitro fertilisation (IVF), sperm function tests may also be performed. Sometimes a test called cryosurvival is done to see how well semen will survive frozen for periods of time, if a couple would like to store sperm for future pregnancies. Investigations to rule out bacterial and viral infections may also be requested by your doctor.
How is it used?
Semen analysis is used to determine whether a man might be infertile (unable to get a woman pregnant). The semen analysis tests many aspects of the semen and sperm. Semen analysis to determine fertility should be performed on a minimum of two samples at least seven days apart over a period of two to three months because some medical conditions can affect sperm levels.
The semen analysis can also be used to count sperm after a man has a vasectomy. If there are still a lot of sperm present in the semen, the man and his partner will have to take precautions so that his partner will not become pregnant. He will have to return for one or more sperm counts until the sperm are cleared from his sample(s).
When is it requested?
Semen analysis is recommended following a vasectomy or testing for infertility. At least 20% of married couples experience problems conceiving, and this is due to the male partner in about 40% of cases. Male infertility has many causes and some of these, such as varicocoele (hardening of the veins draining the testes), can be treated successfully. If male factors are involved, analysis of the semen is necessary to determine the feasibility of using IVF to facilitate pregnancy.
What does the result mean?
The typical volume of semen collected is around a teaspoonful (2-6 millilitres) of fluid. Less semen would indicate fewer sperm, which would affect fertility. More semen indicates too much fluid, which would dilute the sperm, also impeding fertility.
Sperm concentration (also called sperm density) is measured in millions of sperm per millilitre of semen. Levels greater than or equal to 20 million per millilitre (and more than 80 million sperm in one ejaculation) are considered normal. The fewer sperm a sample has, the less chance a man has of getting his partner pregnant. Following a vasectomy the aim is to have no sperm detected in the semen sample.
The percentage of moving sperm in a sample is known as its 'motility'. The more slowly moving or immobile sperm in a sample, the less likely it is that a man could conceive a child with his partner. The progression of the sperm is rated on a basis from zero (no motion) to 3 or higher for sperm that move in a straight line with good speed. If less than half of the sperm are moving, a stain is used to identify the percentage of dead sperm. This is called a 'sperm viability test'.
Morphology analysis is the study of the size, shape and appearance of the sperm cells. The analysis evaluates the structure of 200 sperm and any defects are noted. The more abnormal sperm that are present, the lower the likelihood of fertility.
Is there anything else I should know?
For fertility testing, a man should abstain from ejaculating for 2- 7 days before the sample is collected. Follow the instructions that are provided to you. For other semen analysis abstinence is not required.
Sperm are very temperature-sensitive. If collection is done at home, the sample should be protected from extremes of temperatures (less than 20°C or more than 40°C). Transport condition can be room temperature, (approximately 21°C) but the sample should be kept close to body temperature prior to delivery e.g. keep it close to your body, inside your jacket or shirt pocket. Never refrigerate the sample. If you are unable to obtain the complete specimen make sure to note that it is a partial collection. Post-vasectomy samples do not need to be examined within 60 minutes.
Several factors can affect the sperm count and other semen analysis values. Alcohol and/or drug use, infectin, physical damage to the testicles, radiation treatment of the testicles, or exposure to certain drugs (such as azathioprine) may all cause issues in sperm function. A man with a higher level of oestrogens may also have a lower sperm count.
Some of the common causes of male infertility are extremely high fever, testicular failure (failure of the testicles to produce sperm), obstruction of the tubes that carry semen to the penis and a less than normal amount of sperm in the sample (oligospermia).
Common questions
Motility (which indicates the percentage of living sperm) and morphology (normal shape of the sperm) are most closely linked with good fertility rates.
If you had a good motility on the first reading, you may have a low sperm count later because of a genital infection or because of an inflamed prostate gland
When a couple cannot become pregnant, it is much easier, less invasive and less expensive for the man to be tested first. A man requires only semen analysis and the samples can be collected and tested very quickly (usually within 3 hours). If the man’s semen is normal, then it makes sense to move ahead with the more invasive and expensive tests for female infertility.
Treatment will depend on the cause. It could include surgery to repair a varicocele or a blockage, hormone injections, or use of assisted reproductive technologies.
What is Pathology Tests Explained?
Pathology Tests Explained (PTEx) is a not-for profit group managed by a consortium of Australasian medical and scientific organisations.
With up-to-date, evidence-based information about pathology tests it is a leading trusted source for consumers.
Information is prepared and reviewed by practising pathologists and scientists and is entirely free of any commercial influence.