What is being tested?
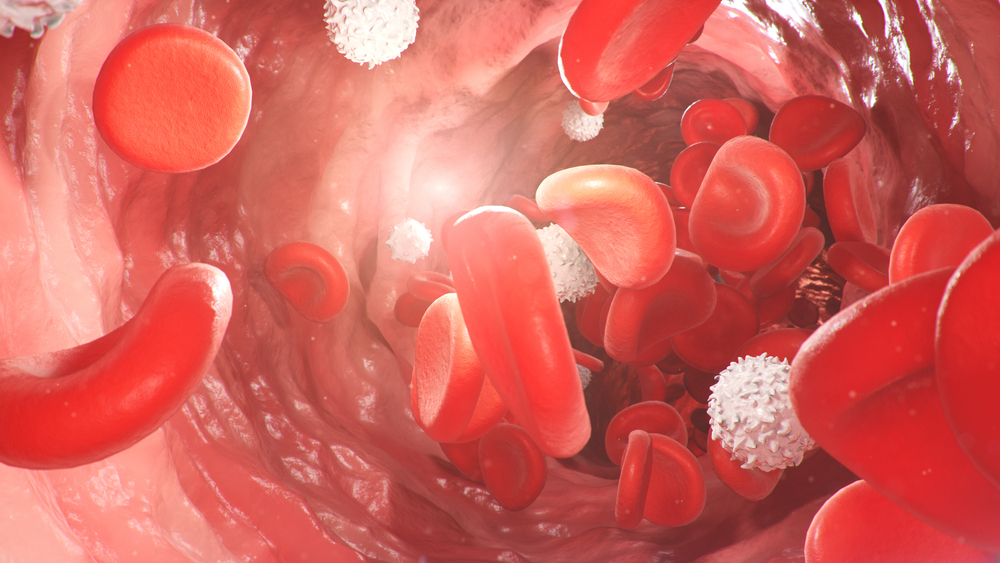
Blood is tested for the presence of haemoglobin S (HbS), which is a genetic variant of the protein haemoglobin. Haemoglobin is found inside red blood cells (RBCs) and is responsible for carrying oxygen from the lungs to all of the tissues and organs of the body.
Normally haemoglobin exists in various forms (haemoglobin A, haemoglobin A2, and haemoglobin F) that are present in different amounts. One genetic abnormality of haemoglobin is known as HbS, which causes the RBC to change shape and affects its ability to carry oxygen. In sickle cell disease, one abnormal HbS gene is inherited from each of the parents.
How is it used?
The test is used to screen for the presence and amount of haemoglobin S (HbS). In the screening test, a chemical is added to the patient's blood sample that reduces the amount of oxygen it carries. In those who carry the sickle cell gene, the reduced amount of oxygen will cause crystals to form. These crystals alter the shape of the RBC, resulting in the characteristic sickle shape. To confirm and identify the amount of HbS present a test is used that separates out the different types of haemoglobin. Each type of haemoglobin will form a unique 'pattern' so that HbS can be identified and a diagnosis of sickle-cell disease made.
When is it requested?
Because sickle cell disease is a genetically inherited disorder, an individual may have the trait (carry one mutated gene from one parent) or the disease (carries two mutated genes, one from each parent), thus the screening test is often performed on infants and children. If you are of African ancestry (about 25% of Africans carry at least one gene for this trait), you may wish to be tested prior to starting a family.
What does the result mean?
If the screening test is negative, it means that the gene for sickle cell trait is not present. If the screening test is positive, then further haemoglobin testing must be performed to confirm whether one mutated gene or both are present. In unaffected individuals HbS is not present. In those who have sickle cell trait, 20% to 40% of the haemoglobin is HbS. In sickle cell disease, as much as 80% to 100% of the haemoglobin may be HbS.
In general, individuals who have sickle cell trait do not have any significant symptoms and live a normal life. Those individuals who carry both abnormal genes have sickle cell disease. In this condition the person may not experience any symptoms under 'normal' conditions, but may experience episodes called 'sickling crises' brought on by, for example, infection or dehydration. During such episodes symptoms can include joint pain, abdominal pain, fever and seizures. In the long-term, sufferers may may experience haemolytic anaemia (breakdown of red blood cells), growth impairment, jaundice and increased risk of serious infections.
Is there anything else I should know?
Because of the abnormal (sickle-cell) shape of the RBC in sickle cell disease, RBCs can become stuck in small capillary blood vessels, thereby blocking the blood supply to various organs. About 25 percent of the African population carry at least one abnormal gene although only a small proportion of these carry both genes. A sickle cell test can screen for presence of the abnormal gene.
The test can fail to detect haemoglobin S (sickle cell disease or trait) under the following circumstances:
Because of the severity of the disease, people of African ancestry who are planning to have children may wish to seek counselling from their doctor to ensure that neither carries the sickle cell trait.
Common questions
The life span of a patient with sickle cell disease has increased significantly to over 50 years of age. Common causes of death include infections, clots or blockages of blood vessels, and kidney failure. There is no cure for sickle cell disease. Treatment is based on the symptoms existing at the time of a 'sickling-crisis'. This may include blood transfusions, antibiotics, on-going fluid intake through intravenous (IV) solutions and/or drinking of fluids, and medication to reduce pain. Red blood cell exchange has been used in sickle cell crisis. More recently, bone marrow transplants have been shown to be effective.
Patients with sickle cell trait generally do not require any long-term treatment. Under certain circumstances, those individuals with the trait who are exposed to reduced levels of oxygen (excessive exercise or high altitudes) may experience some 'crisis-like' symptoms like pain or difficulty breathing.
The sickle cell gene is found mainly among African descendents. Individuals who have sickle-cell trait (i.e. only one copy of the faulty gene) are naturally 'protected' against the parasite that causes malaria, which is why the gene has 'survived' to be passed down through generations. The trait also appears in individuals from the Mediterranean coastal areas and may be seen in those from inter-race backgrounds.
Antenatal testing (i.e. testing the foetus while still in the womb) is available. Amniotic fluid may be tested at 14-16 weeks to provide a definitive answer as to whether or not the foetus has sickle-cell trait or disease. Potential parents can also be tested to see if they carry the sickle-cell gene before starting a family - genetic counselling is strongly encouraged if a positive sickle screen is obtained from one or both parents.
What is Pathology Tests Explained?
Pathology Tests Explained (PTEx) is a not-for profit group managed by a consortium of Australasian medical and scientific organisations.
With up-to-date, evidence-based information about pathology tests it is a leading trusted source for consumers.
Information is prepared and reviewed by practising pathologists and scientists and is entirely free of any commercial influence.