What is being tested?
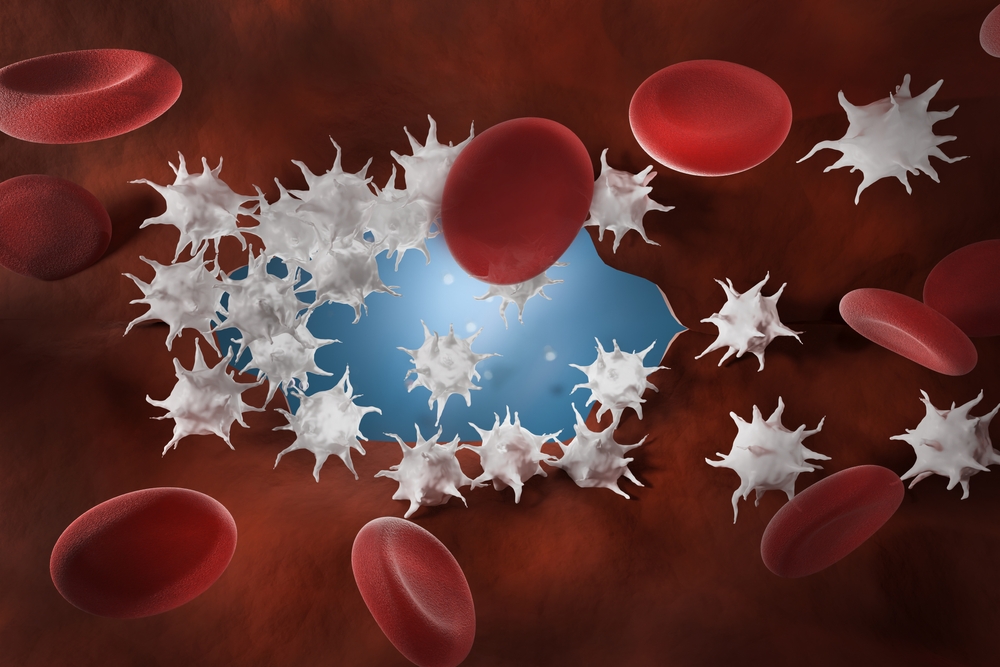
Platelets (thrombocytes) are tiny cells derived from very large cells called megakaryocytes that are made in the bone marrow. These cells (about 2-3 microns in diameter) are released from the bone marrow to circulate in the blood. They are the first components to be activated when there has been an injury to a blood vessel or tissue. They transform in shape and become very sticky and begin the formation of a 'blood clot'. The platelet count is a test that determines the number of platelets in your blood.
How is it used?
Abnormally low platelet counts or abnormally functioning platelets are associated with bleeding disorders or bone marrow diseases, such as leukaemia. These conditions require the determination of the number of platelets present and/or their ability to function correctly.
When is it requested?
A platelet count is often requested as a standard part of a full blood count which may be done as part of an annual examination. It is almost always ordered when a patient has unexplained bruises or takes what appears to be an unusually long time to stop bleeding from a small cut or wound.
What does the result mean?
In an adult, a normal count is about 150-400 x 109 per litre of blood.
If platelet levels fall below 20 x 109/L, spontaneous bleeding may occur and is considered a life-threatening risk. Patients who have a bone marrow disease, such as leukaemia or other cancer in the bone marrow, often experience excessive bleeding due to a significantly decreased number of platelets (thrombocytopenia). As the number of cancer cells increases in the bone marrow, normal bone marrow cells are crowded out, resulting in fewer platelet-producing cells.
Low number of platelets may occur in some patients with long-term bleeding problems (e.g., chronic bleeding stomach ulcers), thus reducing the supply of platelets. Decreased platelet counts may also be seen in patients with Gram-negative sepsis.
Individuals with an autoimmune disorder (such as lupus or idiopathic thrombocytopenia purpura (ITP), where the body's immune system can produce antibodies against platelets may cause the destruction of platelets. Patients undergoing chemotherapy may also have a decreased platelet count from suppression of the bone marrow.
Certain drugs, such as quinine, quinidine, sulpha drugs, digoxin, vancomycin, and valium are just a few that have been associated with drug-induced decreased platelet counts. Patients undergoing chemotherapy or radiation therapy may also have a decreased platelet count. Up to 5% of pregnant women may experience thrombocytopenia at term called gestational thrombocytopenia.
Platelet consumption may be observed in renal diseases. Thrombotic, thrombocytopenic purpura (TTP) and haemolytic uremic syndrome (HUS) are seen in renal failure and can result in fewer circulating platelets in the blood. Similarly, a condition known as splenic sequestration, where platelets pool within an enlarged spleen, can also cause a platelet decrease.
Reticulated platelets: Certain dyes that stain young and old platelets differently or measuring platelet size may be used to assess the number of young platelets and a number of automated cell counters have this facility. This is used as an indication of bone marrow output of platelets. For example, in autoimmune thrombocytopenia there is increased bone marrow output of platelets and increased young (reticulated} platelets are seen in the circulation. This may be used as a help in diagnosing the cause of a low platelet count.
More commonly (up to 1% of the population), easy bruising or bleeding may be due to an inherited disease called von Willebrand's disease. While the platelets may be normal in number, their ability to stick together is impaired due to a decrease in von Willebrand's factor, a protein needed to initiate the clotting process. Many cases may go undiagnosed due to the mild nature of the disease. Many cases are discovered when a patient has to have surgery or a tooth extraction or when delivering a baby. However, some cases are more severe and can be aggravated by use of certain drugs, resulting in a life-threatening situation.
Increased platelet counts (thrombocytosis) may be seen as a reactive response to an inflammatory stimulus or to bleeding, while other people may have a more significant blood problem called myeloproliferative disorder. Some, although they have an increased number of platelets, may have a tendency to bleed due to the lack of stickiness of the platelets; in others, the platelets retain their stickiness but, because they are increased in number, tend to stick to each other, forming clumps that can block a blood vessel and cause damage, including death (thromboembolism). Drugs such as aspirin are used to inhibit this stickiness.
Is there anything else I should know?
Living in high altitudes, strenuous exercise, and being post partum may cause increased platelet levels.
Decreased levels may be seen in women before menstruation.
Drugs that may cause increased platelet levels include oestrogen and oral contraceptives.
Other inherited disorders caused by defective platelets or decreased/absent proteins that activate the platelets include Glanzmann’s Thrombasthenia, Bernard-Soulier disease, Chediak-Higashi syndrome, Wiskott-Aldrich syndrome, May-Hegglin syndrome, and Down syndrome. The occurrence of these genetic abnormalities, however, is very rare.
Common questions
The underlying cause of the bleeding must be determined first and treated. Platelet concentrates may be transfused to increase the number of circulating platelets. In some where there is autoimmune platelet destruction the use of steroids may stimulate an increase in platelet production.
Bruising for no apparent reason, bleeding from the nose, mouth, or rectum also without obvious injury, or the inability to stop a small wound from bleeding within a reasonable period of time, large numbers of pinpoint dots of blood (petechiae) or larger flat collections of blood (purpura) under the skin, may all indicate a platelet deficiency.
Elevated platelet levels where there is a reactive cause usually cause no problems but where there is platelet dysfunction in a myeloproliferative disorder this can lead to blood clots, or paradoxically abnormal bleeding. The greater danger is bleeding that will not stop, or continues for an abnormally long time, due to a low platelet count.
Platelets survive about 8-10 days. If you ingest any aspirin products within this period before surgery platelet function may be diminished resulting in excessive bleeding. Consequently, surgery may be cancelled.
Platelet counts can vary throughout the course of the day; however, counts are highest at midday. Under certain conditions platelets may clump and falsely appear to be low in number.
More information
What is Pathology Tests Explained?
Pathology Tests Explained (PTEx) is a not-for profit group managed by a consortium of Australasian medical and scientific organisations.
With up-to-date, evidence-based information about pathology tests it is a leading trusted source for consumers.
Information is prepared and reviewed by practising pathologists and scientists and is entirely free of any commercial influence.