Summary
What is cholesterol?
If you are being investigated to see if you have familial hypercholesteraemia (FH) and you are the first person in your family to be tested, you will have had several lipid profile tests that have consistently shown that you have high levels of low-density lipoprotein (LDL) cholesterol.
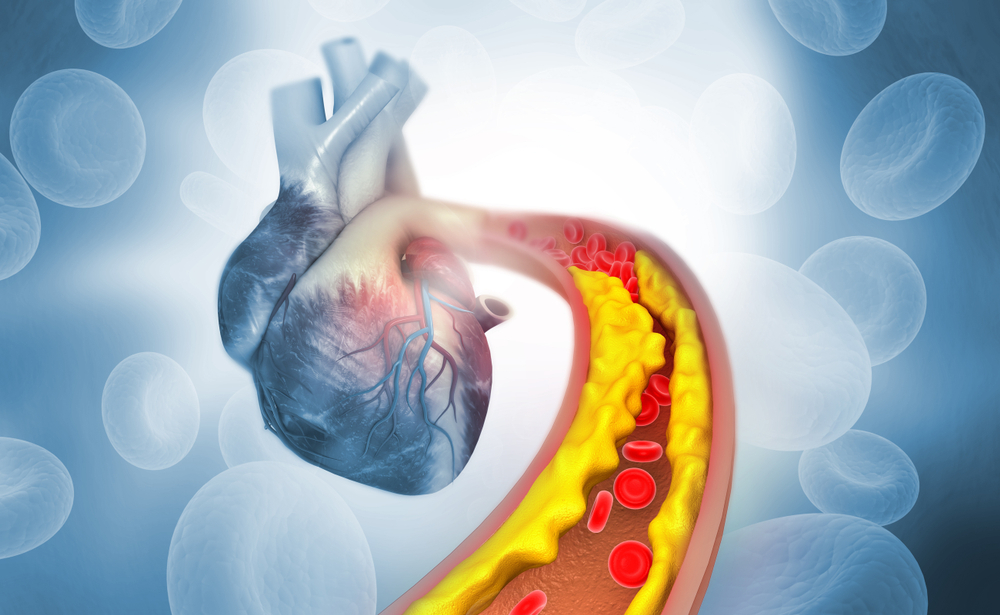
The lipid profile is a common test that is used to assess your risk of heart disease, heart attack or stroke. It measures different types of cholesterol together with triglycerides (another important form of fat) in a sample of your blood. Cholesterol and triglycerides are lipids, or fats. Having too much LDL-cholesterol can put you at risk of developing atherosclerosis – a buildup of plaque in your arteries and blood vessels. This is also sometimes called cardiovascular disease or CVD.
What are lipoproteins
Cholesterol and triglycerides cannot be dissolved in water and need help to move through the blood, as blood is a liquid. They are processed in the liver where they are packaged up with proteins into lipoproteins. This enables them to move through blood rather than rising to the top, like oil on water. In this way, they travel to organs and tissues when and where they are needed.
There are different types of lipoproteins depending on the amounts of fat and protein they contain. They are termed high-density lipoprotein (HDL) and low-density lipoprotein (LDL). There are also different subtypes of lipoproteins such as very low-density lipoprotein (VLDL) and intermediate density lipoprotein (IDL). In general, lipoproteins with a higher fat content and lower protein content (e.g. lower density such as LDL or VLDL) are more likely to stick to artery walls and cause a buildup of plaques.
Although lipids are essential for many of your body’s functions, having too much of low-density types of lipoproteins in your blood is harmful. Your body has systems in place for getting rid of excess lipids but sometimes these systems don’t work as they should, or they become overloaded. Some people have inherited conditions that cause them to have too much low-density lipoproteins.
When you have high amounts of cholesterol and triglycerides circulating in your blood packaged up in low-density lipoprotein, they stick together with other fats, cells, calcium and debris floating around in the bloodstream and form plaques in the walls of arteries. The buildup of plaque narrows the space within the artery. For more on plaque formation and lipoproteins see Lipid Profile.
What is FH?
FH is an inherited disorder, which causes very high LDL cholesterol from birth and will continue to do so throughout life unless it is diagnosed and treated. If you have FH, you can develop atherosclerosis – a build-up of plaque in your arteries and blood vessels – from an early age.
Having the test
Sample
Blood.
Any preparation?
None.
Your results
Possible outcomes of your FH tests This may be because your high cholesterol is: This result does not mean that you do not have FH, just that it cannot be confirmed by genetic testing at this time.A disease-causing (pathogenic), or likely disease-causing (likely pathogenic) gene variant (mutation) is identified. This confirms a diagnosis of FH. A disease-causing variant (mutation) was not identified. A gene variant (mutation) of uncertain significance is identified. This means that based on current knowledge of the gene involved, the laboratory is unable to determine whether the genetic change is the cause of your high cholesterol.
Family testing
If you have FH confirmed by genetic testing and you are the first person in your family to be diagnosed, you are termed an ‘index case’. Each of your close family members – parents, siblings, and children – has a 50 per cent chance of also having the gene variant causing FH and they should be tested. The diagnosis of FH in children should ideally occur before they are 10.
Questions to ask your doctor
The choice of tests your doctor makes will be based on your medical history and symptoms. It is important that you tell them everything you think might help.
You play a central role in making sure your test results are accurate. Do everything you can to make sure the information you provide is correct and follow instructions closely.
Talk to your doctor about any medications you are taking. Find out if you need to fast or stop any particular foods or supplements. These may affect your results. Ask:
More information
Pathology and diagnostic imaging reports can be added to your My Health Record. You and your healthcare provider can now access your results whenever and wherever needed.
Get further trustworthy health information and advice from healthdirect.
What is Pathology Tests Explained?
Pathology Tests Explained (PTEx) is a not-for profit group managed by a consortium of Australasian medical and scientific organisations.
With up-to-date, evidence-based information about pathology tests it is a leading trusted source for consumers.
Information is prepared and reviewed by practising pathologists and scientists and is entirely free of any commercial influence.