Summary
What are lipoproteins?
Cholesterol and triglycerides are fats and therefore cannot be dissolved in water. They need help to move them through the blood, as blood is a liquid, and so are processed in the liver where they are packaged up with proteins into round particles called lipoproteins. This enables it to move through blood rather than rising to the top, like oil on water. In this way, they travel to organs and tissues where and when they are needed for energy or storage.
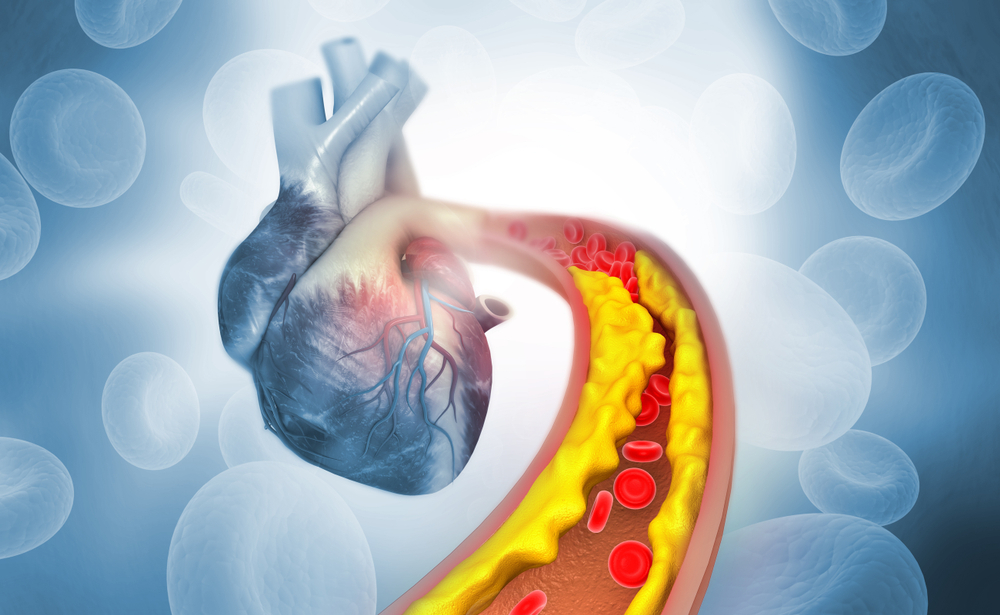
There are different types of lipoproteins depending on the amounts of fat and protein they contain. They are termed high-density lipoprotein (HDL) and low-density lipoprotein (LDL). There are also different subtypes of lipoproteins such as very low-density lipoprotein (VLDL) and intermediate density lipoprotein (IDL). In general, lipoproteins with a higher fat content and lower protein content (e.g. lower density such as LDL or VLDL) are more likely to stick to artery walls and cause a buildup of plaques (this is called atherosclerosis or cardiovascular disease (CVD).
Although lipids are essential for many of your body’s functions, having too much of the low-density types of lipoproteins in your blood is harmful.
When you have high amounts of cholesterol and triglycerides circulating in your blood packaged up in LDL, sometimes called LDL-cholesterol, they stick together with other fats, cells, calcium and debris floating around in the bloodstream and form plaques in the walls of arteries . The buildup of plaque narrows the space within the artery. For more on this see Lipid Profile.
Your body has systems in place for getting rid of excess lipids but sometimes these systems don’t work as they should, or they become overloaded. Some people inherit genetic conditions that cause them to have too much LDL.
What is Lp (a)?
The protein parts of a lipoprotein are referred to apolipoproteins. This is a broad term for the protein in a lipoprotein. Lipoprotein (a) or Lp(a) is a type of lipoprotein very similar to LDL but contains an additional protein called apolipoprotein(a). Higher levels of Lp(a) in the blood are a risk factor for the buildup of plaque in arteries (atherosclerosis). For more on this see the Apo A-1 test.
The amount of Lp(a) in your blood is decided by the genes you inherit from your mother and father. This means lifestyle changes such as diet and exercise do not reduce Lp(a) levels, and most of the commonly used medications to lower LDL-cholesterol are ineffective. Statins do not reduce Lp(a) and may even cause a slight increase. Niacin (vitamin B3) can provide modest reductions, but studies have shown it may cause serious side effects in some people.
Why get tested?
Lp(a) is not included in the Lipid Profile group of tests that is routinely used to assess CVD risk. However, your medical team may request it to help measure your risk if you have a strong family history of heart attack at a relatively young age.
Sometime Lp(a) is ordered if someone has been diagnosed with heart disease or other vascular diseases, especially if the results of routine tests are not abnormal. Many people who have heart attacks have normal cholesterol levels, so doctors are starting to look at other factors that may have an influence on heart disease, such as high Lp(a) levels.
Having the test
Sample
Blood.
Any preparation?
Lp(a) can be measured using a fasting or a random blood sample:
Your results
A high Lp(a) level may increase your risk of developing atherosclerosis – a buildup of plaque in your arteries and blood vessels.
The Lp(a) level tends to remain relatively constant over a person’s lifetime. People also develop a high level of Lp(a) with:
Having a low level of Lp(a) does not appear to cause health problems.
Typically, Lp(a) levels are only tested once because they are usually constant. Occasionally, your doctor may order a second Lp(a) to confirm the initial test result or to see if your risk has increased significantly after menopause or to monitor the effects of treatment.
There is another lipid test known as apolipoprotein A-1 (Apo A-1). This is a different test that is related to HDL or “good” cholesterol.
Questions to ask your doctor
The choice of tests your doctor makes will be based on your medical history and symptoms. It is important that you tell them everything you think might help.
You play a central role in making sure your test results are accurate. Do everything you can to make sure the information you provide is correct and follow instructions closely.
Talk to your doctor about any medications you are taking. Find out if you need to fast or stop any particular foods, medications or supplements. These may affect your results. Ask:
More information
Pathology and diagnostic imaging reports can be added to your My Health Record.
You and your healthcare provider can now access your results whenever and wherever needed. Get further trustworthy health information and advice from healthdirect.
What is Pathology Tests Explained?
Pathology Tests Explained (PTEx) is a not-for profit group managed by a consortium of Australasian medical and scientific organisations.
With up-to-date, evidence-based information about pathology tests it is a leading trusted source for consumers.
Information is prepared and reviewed by practising pathologists and scientists and is entirely free of any commercial influence.