What is being tested?
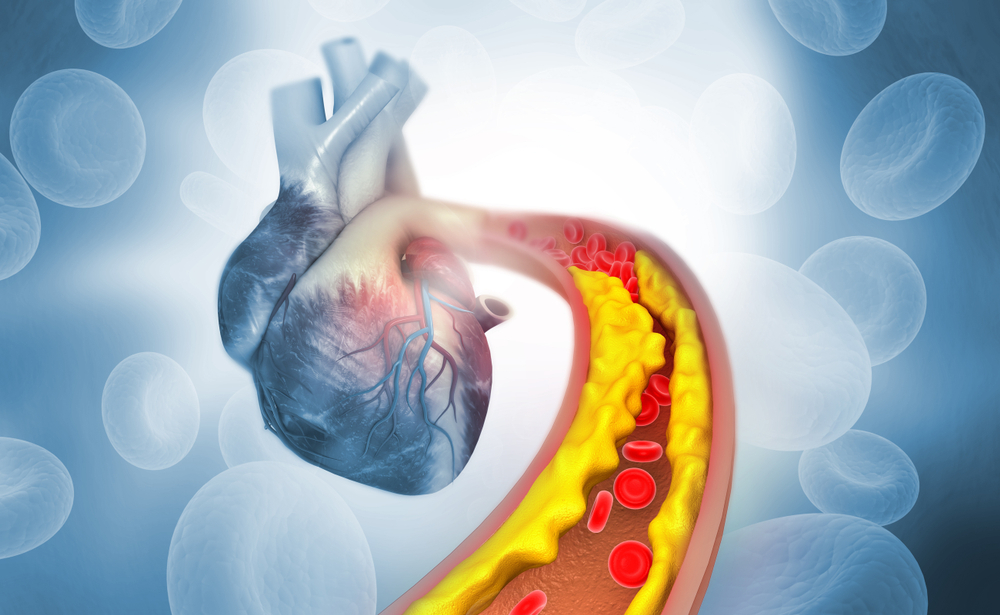
Low-density lipoprotein (LDL) is a type of lipoprotein that carries cholesterol in the blood. The test for LDL cholesterol (LDL-C) measures the amount of cholesterol bound to LDL in the blood. LDL cholesterol is considered to be undesirable because it deposits excess cholesterol in the walls of blood vessels and contributes to 'narrowing of the arteries' (atherosclerosis) which may lead to conditions such as angina, heart attack and strokes. Hence LDL cholesterol is often termed 'bad' cholesterol. The test for LDL cholesterol measures the amount of cholesterol bound to LDL in blood.
LDL-C is usually not measured directly, but calculated by an equation which uses the other components of the lipid profile. Occasionally LDL-C can be measured directly. This test is known as direct LDL and is described separately.
How is it used?
The test for LDL cholesterol is used to predict your risk of developing cardiovascular diseases such as coronary heart disease and stroke. LDL cholesterol is part of the cardiovascular risk assessment. Results of the LDL cholesterol test and other components of the lipid profile are considered along with other risk factors to assess an individual’s risk of developing cardiovascular disease in the next 5 or 10 years. Decisions can then be made about whether treatment is required to lower this risk.
Treatment options may include lifestyle changes such as diet or exercise programs or lipid-lowering drugs such as statins. The treatment target for LDL cholesterol is usually <2.0 mmol/L. although your doctor may decide that a different target is more appropriate for you.
Once a patient has been diagnosed with high LDL cholesterol and has been started on treatment, it will be measured more frequently to assess the response to treatment.
When is it requested?
LDL cholesterol levels are ordered as part a lipid profile, along with total cholesterol, HDL cholesterol (HDL-C), and triglycerides. This profile may be used as a screening test in a healthy person as part of a routine health check, for Aboriginal and Torres Strait Islander adults aged 35 years and over and otherwise adults aged 45 years and over. If the individual is considered to be low risk, the LDL-C should be remeasured in 5 years. Individuals at moderate or high risk require more frequent retesting.
A lipid profile may be requested on someone who has had a high total cholesterol to see if the total cholesterol is elevated because of too much LDL-C. A lipid profile may also be requested in individuals who have one or more major risk factors for cardiovascular disease regardless of their age.
LDL-C may also be requested at regular intervals to evaluate the success of lipid-lowering lifestyle changes such as diet and exercise or to determine the effectiveness of cholesterol-lowering drugs such as statins.
LDL-C may be falsely decreased if you are acutely unwell at the time of measurement (for example, if you have an infectious disease, if you are recovering from a heart attack or have recently had surgery). A lipid profile should be measured once you have recovered from this illness.
What does the result mean?
A high LDL-C is associated with an increased risk of cardiovascular disease. Because LDL-C is only one component of the cardiovascular risk assessment (which takes into account many other factors such as smoking status, family history and blood pressure), the LDL-C result which is considered “high” will vary from person to person. However, in general, an LDL cholesterol above 3.0mmol/L is associated with a potentially increased risk.
If you are on treatment, it is common to aim for an LDL-C below 2.0mmol/L, however your doctor may pick a more appropriate treatment target based on your own individual circumstances. It is important to remember that any reduction in LDL cholesterol reduces cardiovascular risk, even if you do not meet your treatment target.
Those with LDL-C above 5.0mmol/L [ST1] should be reviewed with regards to whether they may have familial hypercholesterolaemia (see below).
If your lipid levels are mildly abnormal, a second confirmatory sample may be taken on a separate occasion before a definitive diagnosis is made as the amount of cholesterol in the blood does vary a little from day-to-day.
Is there anything else I should know?
In most labs in Australia, LDL-C is not actually measured but is calculated from the other results in the lipid profile. This is generally considered accurate, however in a small group of patients with high triglycerides, the calculation is inaccurate and the lab will not be able to report LDL cholesterol. A different test called 'direct LDL-C' is performed in specialised laboratories and gives an accurate LDL-C in these circumstances.
LDL cholesterol should be measured when a person is healthy. LDL cholesterol is temporarily low during acute illness, immediately following a heart attack, or after surgery or an accident. You should wait at least six weeks after any illness to have LDL cholesterol measured.
Cholesterol is high during pregnancy. Pregnant women should wait until at least six weeks after the baby is born before having LDL cholesterol measured.
Common questions
The first step in treating high LDL-C is adoption of lifestyle changes, including decreasing the amount of saturated fat in the diet, achieving and maintaining desirable body weight, and getting regular exercise. If lifestyle changes do not adequately lower LDL-C, drugs such as statins may be prescribed. For people with certain combinations of risk factors and LDL-C levels, drug therapy may be prescribed in concert with lifestyle changes.
Adoption of a diet low in saturated fat (less than 6% of calories from saturated fat) will usually lower LDL cholesterol by about 10%.
Children who have a family history of very high LDL cholesterol or premature cardiovascular disease (generally considered to be a first-degree relative with heart attack or stroke before age 55 if male, or 60 if female) should have a lipid profile once they reach 5 years of age. This is because these patients may have an inherited condition such as familial hypercholesterolaemia (see below) which will benefit from early treatment.
More information
What is Pathology Tests Explained?
Pathology Tests Explained (PTEx) is a not-for profit group managed by a consortium of Australasian medical and scientific organisations.
With up-to-date, evidence-based information about pathology tests it is a leading trusted source for consumers.
Information is prepared and reviewed by practising pathologists and scientists and is entirely free of any commercial influence.