Summary
What tests will you have if you have clotting or bleeding problems?
If your medical team suspects you may have a clotting or bleeding problem one or both of two tests are usually ordered. These are:
It is likely that you will also have a Full blood count.
If the results of these tests are not normal, a range of different tests can be used to gain further information. The choice of tests will depend on what your medical team is investigating but you could expect to have some of these tests:
Other tests that are often done at the same time include:
Why get tested?
Your medical team may request a coagulation profile:
Conditions that cause bleeding or clotting problems include:
There are several rare inherited disorders that affect clotting. Testing is done if an inherited factor deficiency is suspected, especially when bleeding episodes begin early in life or when a close relative has been diagnosed with an inherited factor deficiency.
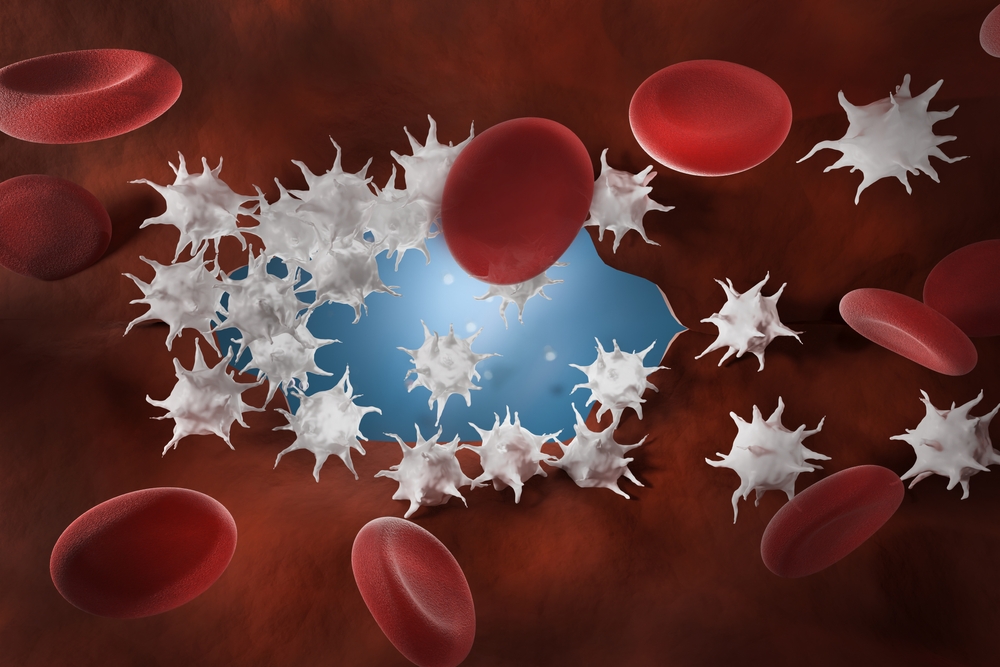
How blood clotting works
Coagulation (blood clotting) factors
Your liver makes most of your coagulation (clotting) factors. Coagulation factors have names, such as fibrinogen and prothrombin. Each factor has been given a number, a Roman numeral, such as coagulation factor I or II or VIII. For more information on coagulation factors and how they make blood clots, go to Coagulation (blood clotting) factors.
What is the coagulation profile?
A typical coagulation profile
The coagulation profile will typically include some of these tests, but which tests will depend on your clinical history and depend on what your medical team is investigating.
| APTT (Activated partial thromboplastin time) | The APTT checks how well most of your coagulation factors work. An abnormal APTT can indicate deficiencies of coagulation factors XII, XI, IX, VIII, X, V, II (prothrombin) and I (fibrinogen). |
| PT/INR - prothrombin time tests | Prothrombin is factor II and is responsible for making thrombin which helps make the fibrin mesh you need to catch platelets and form clots. An abnormal PT/INR can indicate deficiencies of coagulation factors I, II, V, X, VII or X. |
| Platelet count | This counts the number platelets to make sure you have the right amount. Sometimes the sizes of platelets are measured. Changes in platelet size can indicate the cause of abnormal coagulation. |
| Fibrinogen | Fibrinogen is factor 1. It is the coagulation factor that is converted into fibrin to make the mesh that forms around platelets to make clots. This test shows if you have enough fibrinogen. |
| Thrombin time | This test shows how long it takes to turn fibrinogen into fibrin to make the mesh needed for blood clotting. |
| D-dimer | D-dimer is found in your blood when a blood clot is dissolved. It is normally undetectable and only seen when a clot is breaking down. |
Additional tests | |
| Full blood count | This is a group of tests that counts the number of red cells, white cells and platelets per millilitre of blood. Looked at together, along with your symptoms and medical history, this information helps build a picture of the health of your blood. |
| Liver function tests | Coagulation factors are made in the liver. This group of tests looks for liver damage or disease by measuring the levels of several different substances that are either produced by liver cells as part of their normal function or released into the blood when liver cells are damaged. |
| Kidney function tests | Kidney disease can affect the way your body makes red cells and platelets. |
| Vitamin K | The liver uses vitamin K to produce some of the coagulation factors such as Factors II, VII, IX and X. Normally, vitamin K can be taken in through the diet. The normal flora of the intestine also produces vitamin K. |
Having the test
Sample
Blood.
Preparation
None.
Your results
Your initial PT and APTT results can show whether there is a problem with the coagulation process and where the problem is in the pathway.
The results of these tests will guide your medical team as to whether further testing is required including specialised tests of the individual factors. See Coagulation factors for more details.
Reading your test report
Your results will be presented along with those of your other tests on the same form. You will see separate columns or lines for each of these tests.
Reference intervals
Your results will be compared to reference intervals (sometimes called a normal range).
If your results are flagged as high or low this does not necessarily mean that anything is wrong. It depends on your personal situation. Your results need to be interpreted by your doctor.
Questions to ask your doctor
The choice of tests your doctor makes will be based on your medical history and symptoms. It is important that you tell them everything you think might help.
You play a central role in making sure your test results are accurate. Do everything you can to make sure the information you provide is correct and follow instructions closely.
Talk to your doctor about any medications you are taking including Chinese medicines or supplements. Find out if you need to fast or stop any particular foods, medications or supplements. These may affect your results. Ask:
More information
Pathology and diagnostic imaging reports can be added to your My Health Record. You and your healthcare provider can now access your results whenever and wherever needed.
Get further trustworthy health information and advice from healthdirect.
What is Pathology Tests Explained?
Pathology Tests Explained (PTEx) is a not-for profit group managed by a consortium of Australasian medical and scientific organisations.
With up-to-date, evidence-based information about pathology tests it is a leading trusted source for consumers.
Information is prepared and reviewed by practising pathologists and scientists and is entirely free of any commercial influence.